Clinical image and causes of membranous nephropathy
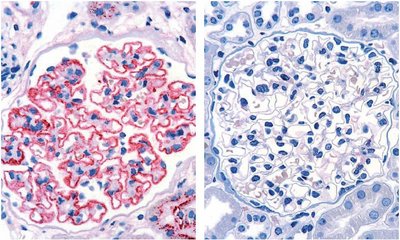
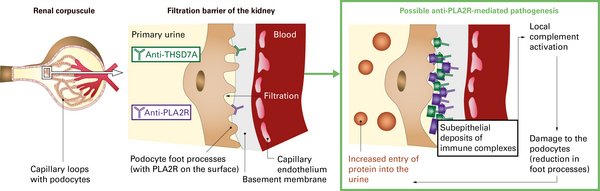
Membranous nephropathy (MN, also membranous glomerulonephritis) is a chronic inflammatory disease of the kidney corpuscles (glomeruli) characterised by thickening of the glomerular capillary walls due to deposits of immune complexes (see illustration). The deposits damage the podocytes and impair the permeability of the glomerular basement membrane in the glomeruli, leading to proteinuria. If protein excretion in the urine increases significantly (>3.5 g/24 h), nephrotic syndrome with reduced protein concentration in the blood (hypoproteinaemia), increased blood lipid levels (hyperlipidaemia) and oedema may develop.1
Approximately 20 to 30% of MN cases occur as secondary conditions as a consequence of different underlying diseases or the use of specific drugs.1,2 They must be differentiated from primary MN, which is caused by autoantibodies (see table). PLA2R and THSD7A are the first antigens to be discovered as target structures of these autoantibodies. If neither an underlying disease nor detectable autoantibodies are present, the condition is referred to as idiopathic MN.3
| Causes of pMN |
|---|
| Autoantibodies (PLA2R/THSD7A) |
| Causes of sMN4 |
|---|
| Infections (e.g. hepatitis B virus, hepatitis C virus, syphilis, malaria) |
| Autoimmune diseases (e.g. rheumatoid arthritis, Sjögren´s Syndrome, bullous pemphigoid) |
| Cancer |
| Other diseases (e.g. sickle cell anaemia, Guillain-Barré syndrome) |
| Drugs (e.g. nonsteroidal anti-inflammatory drugs (NSAID), gold, mercury, penicillamine) |
CONCLUSION: Since the treatment of the two disease forms differs significantly, the diagnostic differentiation between primary and secondary MN is of greatest clinical importance.4 In sMN, the therapy focuses on the underlying disease, whereas patients with pMN are mainly treated with immunosuppressives. Therefore, correct and fast diagnosis may prevent unnecessary diagnostic procedures or drug treatment.
Discovery and pathogenic value of the autoantibodies
In 2009, David J. Salant and colleagues discovered PLA2R, a185-kDa glycoprotein, as a specific autoantigen for antibodies that could be detected in 70-80% of all patients with MN without secondary cause.3 In 2014, a second antigen was described in connection with primary MN, THSD7A.5 The prevalence of antibodies against THSD7A is given with values of up to 10%. Although antibodies against PLA2R and THSD7A can occur in parallel in rare cases, anti-THSD7A antibodies have been found predominantly in anti-PLA2R seronegative pMN patients.6 In patients with sMN, both autoantibodies against PLA2R and THSD7A could not be detected.
The antigens are expressed on the surface of the podocytes. They bind circulating autoantibodies and immune-complex deposits are formed.
The pathogenic mechanism of the development of pMN is not yet fully understood. However, scientists agree that the thickening of the glomerular capillary walls is caused by deposited immune complexes. These trigger local complement activations, which lead to a degradation of the cytoskeleton of the podocytes via the involvement of various mediators. The impaired podocytes lose their filter function and secrete additional factors that have a negative effect on the glomerular basement membrane.1 This causes a progressive impairment of the filter function and thus an increase in the amount of protein in the primary urine (proteinuria). This leads to the development of oedema and a compensatory increase in lipoprotein synthesis, which can result in nephrotic syndrome.
The relevance of autoantibodies in the pathogenesis of pMN was shown in 2017 for THSD7A in the mouse model. Injection of antibodies directed against THSD7A induced severe nephrotic syndrome with proteinuria and hyperlipidaemia in mice.7
While the pathogenesis triggered by the autoantibodies is the same regarding the mechanism, differences have been observed in the clinic of anti-PLA2R and anti-THSD7A-positive pMN patients. A study by Hoxha et al. (2016) showed a higher incidence of malignant tumours in anti-THSD7A-positive patients.8
1Ronco et al., Nat Rev Dis Primers 7, 69 (2021)
2KDIGO, Kidney inter. 100 (Suppl.): 1–276 (2021)
3Beck et al., N Engl J Med 361, 11-21 (2009)
4Trujillo et al., Nephron. 144, 261-271 (2020)
5Tomas et al., N Engl J Med 371, 2277-2287 (2014)
6Tomas et al., J Am Soc Nephrol 28, 3262-3277 (2017)
7Larsen et al., Mod Pathol 29, 421-426 (2016)
8Hoxha et al., J Am Soc Nephrol 28, 520-531 (2017)